Cancer Information
- What is cancer?
- General Cancer Statistics
- cancer types:
- Breast Cancer
- Colorectal Cancer
- Lung Cancer
- Nasopharyngeal Cancer
- Stomach Cancer
- Cancer Prevention
What is cancer?
Cancer is the term for a group of diseases caused by the uncontrolled growth of mutated cells. Cancers are typically named for either the organ where they originated from, or from the type of cells that they mutated from.
According to Center for Health Protection statistics, cancer is the leading single cause of death in Hong Kong. In 2013, an estimated 13,538 individuals died of cancer.
Cancers begin when a cell undergoes a mutation that affects its normal growth and reproduction. While a healthy cell has built in mechanisms that cause it to commit suicide upon cell damage, these mutated cells persist. The result is a buildup of cells where the body does not need, which can create a tumor.
There are two types of tumors, benign and malignant:
· Benign tumors lack the ability to invade adjacent tissues or to spread to distant regions of the body. These are relatively low-risk to one's health, although they still can cause health problems from being a physical mass in the body where one is not supposed to belong.
· Malignant tumors are cancers. These cells can invade other nearby tissues, and if they manage to enter the lymphatic system or the circulatory system (blood vessels) they can spread to distant parts of the body to do more damage. This process is called metastasis. Even when they are removed, malignant tumors can return.
Cancer Staging
Cancer staging describes the severity and extent of a patient's cancer and whether or not it has spread throughout the body. While the process of cancer staging is complicated, it involves the size of the original tumor and whether or not it has penetrated the surrounding tumors, as well as whether or not the cancer has spread to the nearby lymph nodes and to distant parts of the body.
Cancers are typically divided into Stages 0 through 4. A cancer's stage is determined at diagnosis and never changes, even if the disease continues to grow. Stage 0 is the least severe and the easiest, also known as carcinoma in situ, or a small tumor of dysfunctional cells that have not yet become a cancer. On the other hand, a Stage 4 cancer has metastasized and spread to distant parts of the body.
Staging is used by physicians to plan a patient's treatment as well as to determine his or her prognosis, or the likely outcome of the patient's disease. Cancers can typically be cured or managed if they are found at early stages. However, the likelihood of cancer survival falls drastically at higher stages. Most Stage 4 cancers cannot be completely cured by existing treatments.
General Cancer Statistics
In 2011, 26,998 new cases of cancer were diagnosed and 13,241 people died of cancer in Hong Kong, according to the Hong Kong Cancer Registry. Cancer has been the leading cause of death in Hong Kong since the 1980s. While the incidence rate and cancer death rate adjusted by age has decreased somewhat in the past 20 years, cancer remains a serious health burden.
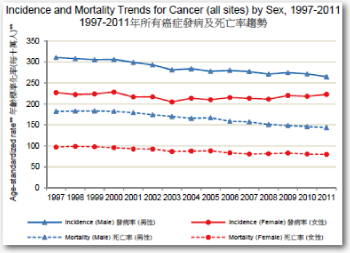
Rates per 100,000 people.
Age adjustment using WHO 2000 World Standard Population
As of 2011, 1 in every 4 men and 1 in every 5 women living in Hong Kong will develop some kind of cancer before they reach the age of 75.
1 in 8 men and 1 in 14 womenin Hong Kong will die of cancer before age 75.
The 10 most common cancers in Hong Kong in 2011 were:
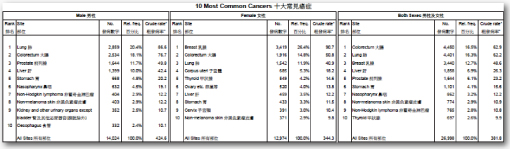
The top ten causes of cancer death in 2011 were
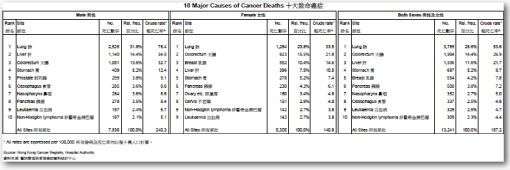
Rates are per 100,000 people
http://www3.ha.org.hk/cancereg/statistics.html
Breast Cancer
Breast cancer is a malignant tumor that starts in the cells of the breast. A malignant tumor is a group of cancer cells that can grow into (invade) surrounding tissues or spread (metastasize) to distant areas of the body. The disease occurs almost entirely in women, but men, in rare occasions, can develop it as well.
Breast cancer is the most common new cancer among women in Hong Kong (90.7 new cases out of every 100,000 people in 2011) and the third most common new cancer among men and women (48.6 cases out of 100,000 people). The risk among women of developing breast cancer is extremely high: 1 in 17 Hong Kong women will develop the disease before the age of 75. Most women who are diagnosed with breast cancer are diagnosed in their middle age, with 57% of incident cases in 2011 being between 40 and 59. However, younger women are still vulnerable, even women in their teenaged years.
Breast cancer is the third leading cause of cancer death among Hong Kong women (14.6 deaths per 100,000 people). Fortunately, due to advanced screening techniques and treatment, breast cancer patients in Hong Kong are fairly likely to survive their cancer. 65% of breast cancers are detected as Stage I or II cancers, where they can be treated more easily.
Common types of breast cancer include –
● Ductal carcinoma – The most common form of breast cancer, which begins in the cells that line the milk ducts in the breast.
● Lobular carcinoma – This kind of cancer begins in the lobules, which are glands in the breast that produce milk.
Symptoms
The symptoms of breast cancer can include:
A change in the shape or size of the breast. These don't necessarily mean cancer. However, women are still encouraged to do a periodic self-exam, and any lumps or irregularities in the breast should be reported to a doctor so breast cancer can be ruled out or diagnosed.
Changes that could indicate cancer are
● A lump or thickening in an area of the breast or a lump or swelling in the armpit.
● A change in the size or shape of a breast
● Dimpling of the skin
● A change in the shape of the nipple, particularly if it turns in, sinks into the breast, or has an irregular shape
● A blood stained discharge from the nipple
● A rash on a nipple or surrounding area
● A lump or thickening in an area of the breast
● Breast Pain
● Redness or an itchy rash around the nipple
Risk Factors for Breast cancer
These factors increase your risk of developing breast cancer.
● Gender - Being a woman is the main risk factor for developing breast cancer. Men can develop breast cancer, but this disease is about 100 times more common among women than men. This is probably because men have less of the female hormones estrogen and progesterone, which can promote breast cancer cell growth
● Aging - Risk of developing breast cancer increases as you get older. About 1 out of 8 invasive breast cancers are found in women younger than 45, while about 2 of 3 invasive breast cancers are found in women age 55 or older.
● Genetic risk factors - About 5% to 10% of breast cancer cases are thought to be hereditary, meaning that they result directly from gene defects inherited from a parent.
■ BRCA1 and BRCA2: The most common cause of hereditary breast cancer is an inherited mutation in the BRCA1 and BRCA2 genes. In normal cells, these genes help prevent cancer by making proteins that keep the cells from growing abnormally. Although in some families with BRCA1 mutations the lifetime risk of breast cancer is as high as 80%, on average this risk seems to be in the range of 55 to 65%. For BRCA2 mutations the risk is lower, around 45%.
◆ Breast cancers linked to these mutations occur more often in younger women and more often affect both breasts than cancers not linked to these mutations. Women with these inherited mutations also have an increased risk for developing other cancers, particularly ovarian cancer.
■ Changes in other genes: Other gene mutations can also lead to inherited breast cancers. These gene mutations are much rarer and often do not increase the risk of breast cancer as much as the BRCA genes. They are not frequent causes of inherited breast cancer.
◆ TP53: The TP53 gene gives instructions for making a protein called p53 that helps stop the growth of abnormal cells. Inherited mutations of this gene cause Li-Fraumeni syndrome (named after the 2 researchers who first described it). People with this syndrome have an increased risk of developing breast cancer, as well as several other cancers such as leukemia, brain tumors, and sarcomas (cancer of bones or connective tissue). This is a rare cause of breast cancer.
◆ PTEN: The PTEN gene normally helps regulate cell growth. Inherited mutations in this gene can cause Cowden syndrome, a rare disorder in which people are at increased risk for both benign and malignant breast tumors, as well as growths in the digestive tract, thyroid, uterus, and ovaries. Defects in this gene can also cause a different syndrome called Bannayan-Riley-Ruvalcaba syndrome that is not thought to be linked to breast cancer risk.
■ Genetic testing: Genetic tests can be done to look for mutations in the BRCA1 and BRCA2 genes (or some other genes linked to breast cancer risk). Although testing may be helpful in some situations, the pros and cons need to be considered carefully. For more information, see the section, "Can breast cancer be prevented?"
● Family history of breast cancer - Breast cancer risk is higher among women whose close blood relatives have this disease. Having one first-degree relative (mother, sister, or daughter) with breast cancer approximately doubles a woman's risk. Having 2 first-degree relatives increases her risk about 3-fold.
● The exact risk is not known, but women with a family history of breast cancer in a father or brother also have an increased risk of breast cancer. Altogether, less than 15% of women with breast cancer have a family member with this disease. This means that most (over 85%) women who get breast cancer do not have a family history of this disease.
● Personal history of breast cancer - A woman with cancer in one breast has a 3- to 4-fold increased risk of developing a new cancer in the other breast or in another part of the same breast. This is different from a recurrence of the first cancer.
● Dense breast tissue - Breasts are made up of fatty tissue, fibrous tissue, and glandular tissue. "Dense breast tissue" (as seen on a mammogram) refers to breasts that have have more glandular and fibrous tissue and less fatty tissue. This has been tied with a greater risk of breast cancer, and also renders make mammograms less accurate.
■ Factors that can affect breast density include age, menopausal status, the use of drugs (such as menopausal hormone therapy), pregnancy, and genetics.
● Being overweight or obese
● Being white
● Alcohol use – The risk increases more with the more drinks that a woman consumes per day. Consuming 2-5 drinks daily leads to 1.5 times the risk compared to nondrinkers.
● Long term use of Hormone therapy (estrogen and progesterone, or a combined therapy)
Protective factors against breast cancer
These factors can reduce your risk of developing breast cancer:
● Keeping a healthy weight
● Exercising regularly
● Limiting your alcohol intake to 1 standard drink (250ml or 3/4 of a can of 5%ABV beer, 100ml or a small glass of 12% ABV wine) per day
Screening for Breast Cancer
As with other cancers, regular screening is necessary to detect There are three tests used to detect breast cancer in women who many not have symptoms yet.
● Mammogram – The mammogram is a test where a breast is compressed between two plates and then X-ray images are taken of it.
■ Mammograms can find extremely small breast tumors that would otherwise be missed by a physical exam. However, they work less well among women who are younger than 50 at finding tumors.
■ Women aged 40 or older are recommended by the American Cancer Society to receive a screening mammogram every year for as long as they are healthy
● Clinical Breast Exam - A clinical breast exam is an exam of the breast by a doctor or other health professional. The doctor will carefully feel the breasts and under the arms for lumps or anything else that seems unusual. It is not known if having clinical breast exams decreases the chance of dying from breast cancer.
● Breast self-exams can be done by women or men to check their breasts for lumps or other changes. It is important to know how your breasts usually look and feel (breast awareness). If you feel any lumps or notice any other changes, talk to your doctor. Doing breast self-exams has not been shown to decrease the chance of dying from breast cancer, and has not been recommended as a screening tool for breast cancer due to the high possibility of unnecessary follow-up medical care..
● MRI in women with a high risk of breast cancer - MRI is a procedure that uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body. This procedure is also called nuclear magnetic resonance imaging (NMRI). MRI does not use any x-rays.
● MRI is used as a screening test for women who have one or more of the following:
■ Certain gene changes, such as in the BRCA1 or BRCA2 genes.
■ A family history (first degree relative, such as a mother, daughter or sister) with breast cancer.
■ Certain genetic syndromes, such as Li-Fraumeni or Cowden syndrome.
● MRIs find breast cancer more often than mammograms do, but it is common for MRI results to appear abnormal even when there isn't any cancer.
Treatment options
● Surgery – Partial (segmental) masectomy or total masectomy
■ Partial masectomy - breast conserving surgery that involves only removing the tumor and the surrounding tissues. Can be called a lumpectomy or a quadrantectomy depending on how much breast tissue is removed. Often followed up with a round of radiotherapy or chemotherapy. This can be a favorable course of action for women with Stage I or II breast cancer.
■ Total masectomy – The entire breast is removed, stopping at the chest wall (pectoral muscles). If it is needed, a radical masectomy will remove the entire breast, some of the closer lymph nodes in the armpit, and might even cut into the chest muscle underneath the breast.
■ Breast reconstruction may be available to restore the shape and contour of the breast, using either implants or the patient's non-breast tissue.
● Radiation Therapy
● Chemotherapy
● Hormone therapy – Blocks the production or activity or certain hormones or hormone receptors that spur cancer cells to grow
● Targeted therapy
◆ Monoclonal antibody therapy – Uses laboratory engineered antibodies that bind with molecules on the surface of cancer cells. The antibodies can bind to and kill cancer cells, slow their growth, trigger an immune response to destroy the cancer cells, or carry toxins or drugs to the cancer cell. Herceptin is a monoclonal antibody in use to treat HER2 positive breast cancer. It seeks out and attaches
◆ Tyrosine Kinase Inhibitor - Tyrosine kinase inhibitors are targeted therapy drugs that block signals needed for tumors to grow. Tyrosine kinase inhibitors may be used with other anticancer drugs as adjuvant therapy.
http://www.cancer.org/cancer/breastcancer/detailedguide/breast-cancer-risk-factors
Cancer Prevention
Tips to reduce your risk for cancer:
1. Do not use tobacco products – Avoid using tobacco products like cigarettes, cigars, or chewing tobacco. Using tobacco increases your risk for cancer of the lung, bladder, kidney cancer, throat, mouth, nasal cavity, esophagus, stomach, pancreas, and cervix, as well as acute myeloid leukemia. Smokers are 15 to 30 times more likely to die of lung cancer than someone who has never smoked.
● Just abstaining from using tobacco is not enough to decrease your risk for cancer. Being exposed to second hand smoke will also increase your risk for lung cancer, and linked to increased risk for lymphoma, leukemia, brain tumors in children, and laryngeal, pharyngeal, nasal, brain, bladder, rectum, stomach, and breast cancer in adults.
● If you smoke, quit smoking. The lungs of former smokers can repair themselves if their owners continue to abstain from smoking.
2. Eat a healthy diet - Although making healthy selections at the grocery store and at mealtime can't guarantee cancer prevention, it might help reduce your risk. Consider these guidelines:
● Eat plenty of fruits and vegetables. Base your diet on fruits, vegetables and other foods from plant sources — such as whole grains and beans.
● Limit fat. Eat lighter and leaner by choosing fewer high-fat foods, particularly those from animal sources. High-fat diets tend to be higher in calories and might increase the risk of overweight or obesity — which can, in turn, increase cancer risk.
● Drink alcohol only in moderation - The risk of various types of cancer — including cancer of the breast, colon, lung, kidney and liver — increases with the amount of alcohol you drink and the length of time you've been drinking regularly.
3. Maintain a healthy weight and be physically active
● Maintaining a healthy weight might lower the risk of various types of cancer, including cancer of the breast, prostate, lung, colon and kidney.
● Physical activity counts, too. In addition to helping you control your weight, physical activity on its own might lower the risk of breast cancer and colon cancer.
● Adults should try to get at least 150 minutes a week of moderate aerobic activity or 75 minutes a week of vigorous aerobic physical activity. You can also do a combination of moderate and vigorous activity. As a general goal, include at least 30 minutes of physical activity in your daily routine — and if you can do more, even better.
4. Protect yourself from the sun
● Protecting yourself from UV radiation from the sun can reduce your risk of skin cancer.
● Wear dark, tightly woven clothing that covers your arms and legs. If you hold your clothing up to the light and can still see through it,
● Wear a hat with a brim of at least 5 to 8 cm. Well designed hats will protect your face, neck, and ears, where many skin cancers form. Also wear sunglasses that are protective against UV rays.
● Apply sunscreen, with at least a Sun Protective Factor of 15, generously to the areas of your body not covered by clothing (face, ears, neck, arms), before spending time in the sun.
■ Broad spectrum sunscreen protects you from both UV-A rays and UV-B rays, where most sunscreens only protect against cancer-causing UV-B rays. Water resistant sunscreens are less likely to wash off in water or sweat. Sunscreen expires after 2 to 3 years
■ Apply sunscreen at least 20 min before you go out into the sun, and reapply sunscreen every 2-3 hours
● Do not use tanning beds or sun lamps
● Stay indoors or in the shade, especially when the sun is highest in the sky (between 10am and 4pm) if possible
5. Get immunized
● Two vaccines for Human Papillomavirus (HPV) types -16 and -18 exist which can reduce a woman's risk of cervical cancer. These are called Cevarix and Gardasil. Gardasil also immunizes against HPV types -6 and -11, and can reduce one's risk for anal and penile cancer.
● The Hepatitis B Virus vaccine can prevent an infection of Hepatitis B, which can lead to liver cancer.
6. Avoid Risky
7. Get regular medical care – Regular self-exams and screenings for various types of cancers, such as skin, colon, prostate, or breast, can help you find cancer at an early stage. Early stage cancer can be treated far more easily than late stage cancer, and the odds of surviving cancer improve drastically the earlier it is detected and diagnosed..
http://www.mayoclinic.org/healthy-living/adult-health/in-depth/cancer-prevention/art-20044816?pg=2
Colorectal Cancer
Colorectal Cancer – Also known as "Bowel cancer", colorectal cancer is a type of cancer that forms in the tissues of the colon (the largest part of the large intestine) or the rectum (last few inches of the large intestine near the anus). The most common colorectal cancers are a certain type of cancer called an adenocarcinoma.
Colorectal cancer is the most common incident (new) cancer in Hong Kong overall, and second most incident cancer for both men and women. 4,450 new cases of colorectal cancer were registered in 2011, with 1,904 deaths from colorectal cancer in that year. There has been a slight upward trend in new colorectal cancer cases in Hong Kong over the last two decades, but this has leveled out since 2001. It is also the second and third leading cause of death from cancer among Hong Kong women and men respectively.
On average, 1 in 22 Hong Kong males will develop colorectal cancer before the age of 75 as will 1 in 35 women.
Signs and Symptoms of Colorectal cancer
Early stage colorectal cancer typically has no symptoms, and many symptoms of later colorectal cancer are also found in patients with non-cancer diseases. However, you should still consult your physician if you experience these symptoms. Even if they turn out not to be cancer, they still could be symptoms of a health problem that needs to be addressed.
● Change in bowel habits — Constipation, diarrhea, narrowing of stools, incomplete evacuation, and bowel incontinence—although usually symptoms of other, less serious problems—can also be symptoms of colorectal cancer.
● Blood on or in the stool — By far the most noticeable of all the signs, blood on or in the stool can be associated with colorectal cancer. However, it does not necessarily indicate cancer, since numerous other problems can cause bleeding in the digestive tract, including hemorrhoids, anal tears (fissures), ulcerative colitis, and Crohn's disease, to name only a few. However, if you notice blood in or on your stool, see your doctor to rule out a serious condition and to ensure that proper treatment is received.
● Unexplained anemia — Anemia is a shortage of red blood cells, the sort that carry oxygen throughout the body. If you are anemic, you may experience shortness of breath. You may also feel tired and sluggish, so much so that rest does not make you feel better.
● Abdominal pain or bloating
● Unexplained weight loss or tiredness
● Vomiting
Screening for Colorectal cancer
As with many cancers, most cancer symptoms don't manifest until the cancer is at a later stage. Screening is important to detect colorectal cancer early while it is still easily treatable. Consult with your doctor to discuss the potential benefits and harms of each test. Standard screening tests for colorectal test are:
● Fecal Occult Blood Test – fecal samples are collected by the patient using a kit, and the stool is examined for traces of blood. FOBT should be performed regularly every one or two years
● Flexible Sigmoidoscopy - For this test, the doctor puts a short, thin, flexible, lighted tube into your rectum. The doctor checks for polyps or cancer inside the rectum and lower third of the colon.
■ How often: Every 5 years with FOBT every 3 years.
● Colonoscopy –This is similar to flexible sigmoidoscopy, except the doctor uses a longer, thin, flexible, lighted tube to check for polyps or cancer inside the rectum and the entire colon. During the test, the doctor can find and remove most polyps and some cancers. Colonoscopy also is used as a follow-up test if anything unusual is found during one of the other screening tests. Requires the colon and rectum to be clean before examination.
■ How often: Every 10 years.
■ A colonoscopy can be very sensitive to tumors and polyps in the colon, but they require an extensive and possibly unpleasant bowel cleansing. While they are generally safe, there is a risk that the procedure may tear the inner wall of the colon and cause bleeding.
● Alternative Screening Methods
■ Virtual colonoscopy – a CT scanner is used to produce high resolution images of the colon and rectum. This has a similar sensitivity (ability to detect polyps and small cancers) to conventional colonoscopy without the attendant complications, but a conventional colonoscopy may be required if polyps or cancer is found.
■ Double Contrast Barium Enema (DCBE) – The patient is given an enema using a barium solution that is drained, leaving a coating of barium on the inner surface of the colon. X-rays are then taken, with the barium making it easier to spot any abnormalities.
● Who should get screened?
■ People who are age 50 or above should consult their physician about colorectal cancer screening.
■ People of average or greater risk for colorectal cancer (see Risk factors for colorectal cancer).
● Further steps if an abnormality is found
■ Further tests may be performed, including x-rays or MRIs of the gastrointestinal tract. If a polyp or tumor is found during a sigmoidoscopy or colonoscopy, a biopsy (retrieval of a tissue sample for lab analysis) or polyectomy (removal of the polyp). Abnormal results from a FOBT will require a colonoscopy.
Risk factors that increase your risk for colon cancer
● Age – Being over 50 increases your risk for colorectal cancer
● Male gender
● Family or personal history of colorectal cancer
● Personal history of inflammatory bowel disease
● Inherited risk factors – Genetic changes linked to familial adenomatous polyposis or Lynch Syndrome (hereditary nonpolyposis colon cancer or HNPCC) can increase one's risk for developing colon cancer
● Alcohol use – Consuming 3 or more alcoholic beverages per day
● Cigarette use
● Obesity increases risk of colorectal cancer and colorectal cancer mortality Protective factors – How can you reduce your risk for colorectal cancer?
● Regular physical activity
● Hormone replacement therapy, either estrogen-only or combination (including estrogen and progesterone), can decrease risk of colorectal cancer in postmenopausal women. However, the evidence behind this is still inconclusive and mixed.
● Polyp removal – Most polyps are adenomas, a benign growth of epithelial tissue of a glandular nature/origin. These can be precursors to colorectal cancer, many of whom are adenocarcinomas (the malignant version of adenomas). Removing these precursor colonic polyps can reduce one's risk of developing colon cancer.
Potential risk and protective factors (inconclusive or mixed evidence)
■ Diet – Red meat, processed meat, cheese, heme iron (a form of iron that is absorbed from animal protein), dietary animal fat and sugars may all increase colorectal cancer risk
◆ Garlic, milk, non-starchy vegetables and fruits, as well as dietary fiber and vitamin D, may possibly decrease colorectal cancer risk.
◆ Other dietary factors (including fish, folate and selenium) have been studied but their relation to bowel cancer risk is not classified by WCRF/AICR because evidence is too limited to draw conclusions.3
■ Nonsteroidal anti-inflammatory drugs - Asprin – Some studies have found that taking Asprin every day for at least 5 years, or every other day for 10 years in women, can reduce one's risk for adenomas (benign tumors) in the colon as well as colorectal cancer. There is weaker evidence that
◆ Heavy Asprin use can cause an elevated risk of bleeding in the gastrointestinal system as well as stroke, and these side effects should be taken into account.
◆ The US Preventive Services Task Force currently recommends against the use of asprin or other NSAIDs at higher than normal doses for extended periods of time, as the potential benefits (decreased risk of colorectal cancer) are outweighed by the potential harms (increased risk of stroke or gastrointestinal bleeding).
Treatment Options
● Surgery is usually performed for early stage colorectal cancer, where the initial tumor can be excised fairly easily. Stage IV (metastasized) cancer is much more difficult to treat with surgery.
■ Local excision – If the tumor is small enough, a doctor insert a tube with a cutting tool through the rectum into the colon to cut the tumor out iwithout damaging a lot of healthy tissue.
■ Resection of the colon with anastomosis – For larger cancers. Doctor will remove the cancer and a small amount of healthy tissue around it. The doctor may then perform an anastomosis (sewing the halthy parts of the colon together). The doctor will also usually remove lymph nodes near the colon and examine them under a microscope to see whether they contain cancer.
■ Resection of the colon with colostomy: If sewing healthy parts of the colon together is not an option, a stoma (an opening) is made on the outside of the body for waste to pass through. This procedure is called a colostomy. A bag is placed around the stoma to collect the waste. This procedure can be temporary or permanent, depending on the patient and the cancer.
● Radiofrequency ablation – A noninvasive therapy where a special probe with electrodes is used to apply heat to the tumor cells, killing them.
● Cryosurgery – A special instrument is used to freeze and destroy tumors.
● Chemotherapy – Chemotherapy uses cell killing (cyto-toxic) drugs that attack rapidly dividing cells, which include cancer cells. Chemotherapy, as opposed to the more recently developed targeted therapy, is systemic, affect cells throughout the entire body. Chemotherapy drugs act on cells that undergo reproduction frequently, which means that cancer cells are targeted. However because these drugs affect cells all around the body, there are many serious side effects associated with chemotherapy which must be accounted for when deciding which treatments to use.
● Radiotherapy – Radiation therapy applies targeted ionizing radiation to the area of the tumor in order to kill tumor cells.
● Cancer treatment plans often include not just one kind of therapy but rather multiple kinds, a process known as combination or multimodality therapy. Doctors may follow up surgery of a locally advanced tumor with chemotherapy in order to make sure that all of the cancer cells are killed off. Alternatively, administering radiation therapy with chemotherapy in advance has been shown to be more effective than just using radiation therapy alone.
http://www.cancer.gov/cancertopics/pdq/treatment/colon/Patient/page4#Keypoint15
http://www.cancer.gov/cancertopics/types/colon-and-rectal
http://www.uspreventiveservicestaskforce.org/uspstf07/aspcolo/aspcolors.htm
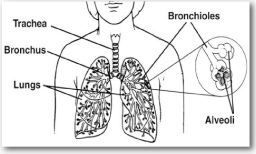
Lung Cancer
Lung cancer is a type of cancer that develops in the lungs, two large, spongy organs found in the chest cavity that are instrumental to the intake and delivery of oxygen to the body's circulatory system. Lung cancer is the leading cause of cancer mortality in the world: 1.3 million people die of lung cancer each year.
Lung cancer was the second most common type of newly diagnosed cancer in Hong Kong in men and women, with 4,401 new cases in 2011. Hong Kong men have a lifetime risk of developing lung cancer before age 75 of 1 in 20, with 1 in 41 women being diagnosed with lung cancer before 75 as well.
It also was the most deadly, having caused 3,789 deaths that year and accounting for 29% of all cancer deaths. 1 in 24 Hong Kong men and 1 in 63 Hong Kong women will die from lung cancer before they reach 75.
There are two main types of lung cancer: small-cell lung cancer and non-small cell lung cancers. About 85-90% of lung cancers are non-small-cell lung cancers. Differentiation between SCLC and NSCLC is done by examining the abnormal cells that make up the cancer. SCLC and NSCLC have different treatment and prognostic profiles.
Using modern medicine, the prognosis for a lung cancer patient is generally poor. The lethality of lung cancer is due to the fact that most lung cancers are not found until they've reached a late stage and have spread throughout the body, as well as the inability to permanently force late stage lung cancer into remission using current medical therapies. Non-small cell cancers tend to have better survival outcomes than small cell lung cancers, but US 5 year survival rates for people diagnosed with Stage IA NSCLC are still under 50%.
Symptoms of Lung cancer
Many lung cancers take time to display symptoms and may not do so until the cancer as advanced. Symptoms of lung cancer that are in the chest: include:
● Coughing, especially if it persists or becomes intense
● Pain in the chest, shoulder, or back unrelated to pain from coughing
● A change in color or volume of sputum
● Shortness of breath
● Changes in the voice or being hoarse
● Harsh sounds with each breath (stridor)
● Recurrent lung problems, such as bronchitis or pneumonia
● Coughing up phlegm or mucus, especially if it is tinged with blood
● Coughing up blood
If the original lung cancer has spread, a person may feel symptoms in other places in the body. Common places for lung cancer to spread include other parts of the lungs, lymph nodes, bones, brain, liver, and adrenal glands. Symptoms of lung cancer that may occur elsewhere in the body:
● Loss of appetite or unexplained weight loss
● Muscle wasting (also known as cachexia)
● Fatigue
● Headaches, bone or joint pain
● Bone fractures not related to accidental injury
● Neurological symptoms, such as unsteady gait or memory loss
● Neck or facial swelling
● General weakness
● Bleeding
● Blood clots
Risk factors and causes for Lung Cancer
● Smoking – Smoking is one of the single greatest risk factors that can increase your risk of developing lung cancer. The risk of lung cancer increases with the more frequently a person smokes cigarettes. On average, a current smoker has 20 times the risk of developing lung cancer than a nonsmoker does.
■ Quit Smoking! (Quit smoking hotline)
● Secondhand smoke – Secondhand smoke is the smoke emitted by burning tobacco as well as the smoke exhaled by a smoker, which is then inhaled by a nonsmoker.
■ Secondhand smoke (SHS) is classified as a "known human carcinogen" (cancer-causing agent) by the US Environmental Protection Agency (EPA), the US National Toxicology Program, and the International Agency for Research on Cancer (IARC – a branch of the World Health Organization).
■ Tobacco smoke is a mixture of gases and particles. It contains more than 7,000 chemical compounds. More than 250 of these chemicals are known to be harmful, and at least 69 are known to cause cancer.
■ There is a large body of research showing that second hand smoke increases a non-smoker's risk of lung cancer by, on average, 20%. There is no safe level of exposure to secondhand smoke.
● Occupational exposure to lung carcinogens – Workplace exposure to asbestos, arsenic, beryllium, cadmium, chromium, and nickel increases lung cancer risk and death rates by over 500% in those who are most exposed compared to those who are not exposed.
● Environmental exposure to radon and air pollution – Air pollution, particularly small particles (fine particulate matter) is tied to an approximately 40% increased risk of lung cancer.
● Being infected with HIV
http://www.cancer.gov/cancertopics/types/lung
● Screening for Lung Cancer
■ Chest x-ray: An x-ray of the organs and bones inside the chest. An x-ray is a type of energy beam that can go through the body and onto film, making a picture of areas inside the body.
■ Sputum cytology: Sputum cytology is a procedure in which a sample of sputum (mucus that is coughed up from the lungs) is viewed under a microscope to check for cancer cells.
■ Low-dose spiral CT scan (LDCT scan): A procedure that uses low-dose radiation to make a series of very detailed pictures of areas inside the body. It uses an x-ray machine that scans the body in a spiral path. The pictures are made by a computer linked to the x-ray machine. This procedure is also called a low-dose helical CT scan.
◆ LDCT scans have been shown to reduce cancer mortality (deaths) in smokers, as unlike Chest X-rays and sputum cytology LDCT can more easily detect early stage cancers.
■ The USPSTF recommends annual screening for lung cancer with low-dose computed tomography (LDCT) in adults aged 55 to 80 years who have a 30 pack-year (that is, to have smoked 1 pack per day for 30 years, 2 packs per day for 15 years, etc.) smoking history and currently smoke or have quit within the past 15 years. Screening should be discontinued once a person has not smoked for 15 years or develops a health problem that substantially limits life expectancy or the ability or willingness to have curative lung surgery.
Treatments for Lung Cancer
Non-Small Cell Lung Cancer
There are nine standard treatments for NSCLC. They are:
● Surgery – A wedge resection is surgery to remove a tumor and a small amount of noramal tissue around it. A segmental resection removes more tissue. If the tumor grows larger, a lobectomy (removal of a lobe, of which there are 3 in the right lung and 2 in the left) or pneumonectomy (removal of the entire lung) may be necessary.
● Radiation therapy or radiotherapy – External radiation therapy
● Chemotherapy
● Targeted therapy –Targeted therapy is a type of treatment that uses drugs or other substances to identify and attack specific cancer cells without harming normal cells. Monoclonal antibodies and tyrosine kinase inhibitorsare two types of targeted therapy being used in the treatment of non-small cell lung cancer.
■ Monoclonal antibody therapy uses antibodies made in the laboratory from a single type of immune system cell. These antibodies can identify substances on cancer cells or normal substances that may help cancer cells grow. The antibodies attach to the substances and kill the cancer cells, block their growth, or keep them from spreading. Monoclonal antibodies are given by infusion. They may be used alone or to carry drugs, toxins, or radioactive material directly to cancer cells.
■ Tyrosine kinase inhibitors are targeted therapy drugs that block signals needed for tumors to grow. Tyrosine kinase inhibitors may be used with other anticancer drugs as adjuvant therapy.
Laser Therapy
● Photodynamic therapy - Photodynamic therapy (PDT) uses a drug (photosensitizer) and a certain type of laser light to kill cancer cells. The drug collects more in cancer cells than in normal cells. Fiberoptic tubes are then used to carry the laser light to the cancer cells, where the drug becomes active and kills the cells. PDT causes little damage to healthy tissue. It is used mainly to treat tumors on or just under the skin or in the lining of internal organs. When the tumor is in the airways, PDT is given directly to the tumor through an endoscope.
● Cryosurgery
● Electrocautery – Uses a probe/needle heated with an electric current to destroy the cancer cells.
http://www.cancer.gov/cancertopics/pdq/treatment/non-small-cell-lung/Patient/page4
Small Cell Lung Cancer
● The standard treatments for Small Cell Lung Cancer are chemotherapy and radiation therapy. These are used in combination with each other and typically cause the cancer to shrink and extend a patient's life. If the cancer is detected at a very early stage where it is fairly small and only in one lung, surgery may be used to remove the tumor and then followed by chemotherapy and radiation therapy. This form of treatment for SCLC is rare and typically not feasible, as the cancer is usually found more advanced and in both lungs.
● Radiation therapy might be applied to the head as a preventative measure, since small cell lung cancer has a high risk of spreading to the head.
Prognosis for lung cancer patients
● Non-Small Cell Lung Cancer
■ Stage 1 – This is the earliest stage and so has the best outcome. Depending on where the cancer is, it is often possible to remove stage 1 lung cancer with surgery. Unfortunately, it is uncommon for lung cancer to be diagnosed this early. Stage 1 non small cell lung cancer is divided into 2 stages, stage 1A and 1B.
◆ Of all the people with stage 1A non small cell lung cancer, between 58% and 73% will live for at least 5 years after diagnosis.
◆ Of all the people with stage 1B non small cell lung cancer, 43% to 58% will live for at least 5 years.
■ Stage 2 – Stage 2 non small cell lung cancer is also divided into stage 2A and 2B.
◆ For stage 2A lung cancer, 36% to 46% will live for at least 5 years with treatment.
◆ For stage 2B non small cell lung cancer, 25% to 36% will live for at least 5 years.
■ Stage 3 – As you might expect, the survival statistics fall with more advanced stages of lung cancer. Again, stage 3 is divided into stage 3A and stage 3B.
◆ For stage 3A non small cell lung cancer, 19% to 24% of patients will live for at least 5 years.
◆ For stage 3B, between 7 and 9 out of every 100 people diagnosed (7% to 9%) will live for at least 5 years.
◆ Stage 4 - is the most advanced stage, where the cancer has spread. Understandably, the survival statistics are very low for this stage. Unfortunately, lung cancer is often diagnosed late and for many people the cancer has already spread when they are diagnosed. Only between 2 and 13 out of every 100 people diagnosed with stage 4 non small cell lung cancer (2% to 13%) will live for at least 5 years. Small cell lung cancer
● Small cell lung cancer
■ Sometimes doctors divide small cell lung cancers into just 2 groups. These are limited disease (the cancer has not spread beyond the lung) and extensive disease (the cancer has spread beyond the lung).
■ Of all the people diagnosed with small cell lung cancer, around 1 in 3 have limited disease at the time of diagnosis. With treatment about 25 out of every 100 people (25%) will live for at least 2 years.
■ 2 out of 3 people with small cell lung cancer already have extensive disease at the time of diagnosis. Unfortunately the survival rate is very low. With treatment, fewer than 5 out of every 100 people (5%) will live for at least 5 years.
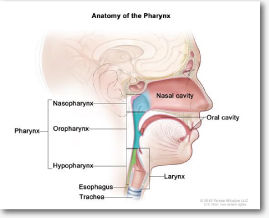
Nasopharyngeal cancer
Nasopharyngeal cancer - Cancer that forms out of tissues in the nasopharynx, the upper most portion of the pharynx which lies directly behind the nose. There are three major types of nasopharyngeal cancer: Keratinized (Type 1) and unkeratinized (Type 2) squamous cell carcinoma, and undifferentiated carcinoma (Type 3). Undifferentiated carcinoma is the most common type of nasopharyngeal cancer that is found in Hong Kong and south Asia.
There are two lymph nodes located extremely close to the nasopharynx. This is a problem for oncologists and patients because cancer can spread to the lymph nodes and undergo regional metastasis.
http://www.cancer.gov/cancertopics/pdq/treatment/nasopharyngeal/Patient/page1
Nasopharyngeal cancer is the 6th most common incident cancer in Hong Kong in men, and the 7th most common overall. 862 new cases of nasopharyngeal cancer were recorded in 2011. Both the incidence and mortality rates of nasopharyngeal cancer in Hong Kong have declined over the past 20 years, but it still ranks 7th in cancer deaths overall as well as among men.
The lifetime risk of developing nasopharyngeal cancer before the age of 75 is 1 in 79 Hong Kong men and 1 in 246 women. The lifetime risk of dying from nasopharyngeal cancer before 75 is 1 in 175 men and 1 in 795 women. Adults in their middle age are at a high risk of being affected by nasopharyngeal cancer, as the median age at diagnosis is around 50 years for both men and women.
Symptoms of Nasopharyngeal cancer
In many cases, patients may not know that they have nasopharyngeal cancer until they feel a lump or mass one or both sides of the neck. This is nasopharyngeal cancer that has invaded the lymph nodes and has advanced to a later stage. However, there are several sign and symptoms that may be found in early stage nasopharyngeal cancer. Most symptoms of nasopharyngeal cancer are shared with other, less serious conditions. However, you should see your physician about these if they persist for more than three weeks.
● Postnasal dribbling
● A nasal obstruction
● A blocked feeling in the ear
● A lump in the nose or neck
● Hearing loss, which is usually only on one side
● Loss of appetite or weight
● Trouble breathing or speaking
● Nosebleeds
Screening for Nasopharyngeal cancer
Screening is necessary to detect nasopharyngeal cancer while it is still at an early stage, where treatment outcomes and survival rates are the best. According to the Hong Kong Anti-Cancer Society, the 5 year survival rates for nasopharyngeal cancer decrease from 90% for patients with Stage I cancer compared to 60% for patients. However, in the absence of screening, only 1 out of 10 patients are diagnosed when their cancer is still Stage 1.
In most countries, where nasopharyngeal cancer is extremely rare, health officials do not usually recommend screening for nasopharyngeal cancer. There is no simple, non-invasive exam or blood test that can reliably find this cancer early. Screening for nasopharyngeal cancer is done in the Hong Kong on an opportunistic basis.
● Epstein-Barr virus serology – Measures a blood sample to check for Epstein-Barr virus antibodies or DNA in the bloodstream. This test screens for the presence of EBV in the patient's body as EBV infection is tied to a higher risk of nasopharyngeal cancer. The test cannot detect nasophayngeal cancer on its own.
● Nasoscopy or upper endoscopy – A thin, flexible tube is inserted in the nose or mouth, respectively, to check for abnormal growths. The nasoscope or endoscope can also be used to retrieve tissue samples for biopsy
Risk Factors
● Gender – Nasopharyngeal cancer occurs twice as often in males compared to females.
● Family history – Family members of people with nasopharyngeal cancer have a higher risk of developing the cancer. It is unclear if this is due to inherited genes, shared environmental exposures (such as shared living spaces), or some combination of these.
● Infection by the Epstein-Barr virus (EBV) – an EBV infection has been associated with nasopharyngeal cancer and benign tumors. The mechanism that links EBV infection with nasopharyngeal cancer is unclear, and while many nasopharyngeal cancer patients have an EBV infection, the vast majority of patients with EBV infections will not develop nasopharyngeal cancer.
● Certain environmental factors
● Living in southern China – While nasopharyngeal cancer is very rare in much of the world (with barely 1 case among every 100,000 people each year), it is significantly more common in southern China, particularly Guangdong Province.
● Heavy alcohol and tobacco use – There is some evidence that heavy alcohol use and smoking contributes to a heightened risk of nasopharyngeal cancer, although the existing research is inconclusive and more research is needed.
● Diet – Is a hypothesized risk factor. Studies have shown that the consumption of salt cured meat and fish or pickled foods, especially when consumed in childhood, can increase the risk of nasopharyngeal cancer later in life.
Protective Factors
● Eliminating certain foods from your diet, including salt cured meat and fish or pickled foods, may decrease your risk for nasopharyngeal cancer.
Treatment methods
■ The standard treatments for nasopharyngeal cancer involve radiation therapy, often given at the same time as chemotherapy. Radiation therapy applies high energy
■ Surgery can be used to remove potentially cancer-compromised lymph nodes. It is rarely used to remove a cancer directly, due to the difficulty of safely accessing the nasopharynx.
■ The success of treatment depends on what type of cells make up the cancer. Type 3 nasopharyngeal cancer, called undifferentiated carcinoma, is the easiest to treat because it is most responsive to chemotherapy and radiation therapy.
● New advances in nasopharyngeal cancer
http://www.cancer.org/acs/groups/cid/documents/webcontent/003124-pdf.pdf
Stomach Cancer
Stomach cancer is a type of cancer that begins in the stomach, an organ in the body that plays a vital role in the breaking down of food so that the nutrients it contains can be absorbed into the body. The stomach lies in the upper part of the abdomen, between the lungs and diaphragm and the small intestine.
Stomach cancer was the 6th most common type of incident cancer in Hong Kong in 2011, accounting for 4.1% of all new cases, being found more in men than in women. There were 1,101 new registered cases of stomach cancer in 2011, with 687 deaths related to stomach cancer. It is also the 4th and 5th leading causes of cancer death among Hong Kong men and women respectively. Stomach cancer incidence and mortality have both declined since 1997.
On average, 1 in 87 Hong Kong men and 1 in 163 women will develop stomach cancer at some point in their lives before they reach the age of 75. The lifetime risk of dying from stomach cancer before the age of 75 is 1 in 169 men and 1 in 282 women. However, stomach cancer patients tend to be older. The median age for stomach cancer diagnoses in 2011 was 71 in men and 70 in women, and the median age at death from stomach cancer was 75 years.
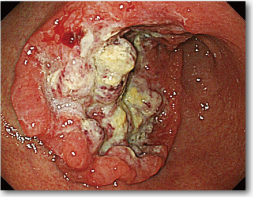
Advanced Type 2 (fungating) stomach cancer as viewed through an endoscope.
Signs and Symptoms of Stomach Cancer
Early stage stomach cancer often has very few symptoms. However, some warning signs do manifest for patients with early stomach cancer. Many of these early symptoms are similar to the symptoms of a peptic ulcer. However, those who experience these symptoms should see their physicians, especially if the symptoms do not go away. Stomach cancer is the most treatable if it is discovered and diagnosed at an early stage, and even if the symptoms do not come from cancer, there could be another health problem that is causing these symptoms.
Symptoms of stomach cancer:
● Indigestion and stomach discomfort – Long term indigestion, acidity, and burping may be a symptom of early stage stomach cancer.
● A bloated feeling after eating
● Mild nausea
● Loss of appetite
● Heartburn
● Abdominal (belly) or stomach pain.
● Weight loss (without trying)
● Low red blood cell count (anemia), feeling faint or lightheaded
Screening for stomach cancer
Screening for cancer is used to detect stomach cancer while it is still at an early stage. Early stage stomach tumors, which are still small and have not yet spread to other parts of the body, are typically treatable, while more advanced cancer generally cannot be cured.
Unlike some other cancers, screening for gastric cancer is uncommon and tends to be done on an opportunistic (patient and general practitioner) basis. Most countries, particularly those in North America and Western Europe, do not encourage systematic screening for stomach cancer because the incidence of stomach cancer in those countries is low. In Japan, where stomach cancer is the most common cancer, a universal gastric cancer screening program has been implemented. Stomach cancer screening in Hong Kong is still done on an individual, case to case basis as decided by a patient and his or her physician. While there are several methods widely used for the screening of stomach cancer, there is only limited evidence that these methods can actually improve an individual's chances of surviving stomach cancer.
Screening methods used to detect stomach cancer include:
● Barium Meal gastric photofluorography – A liquid is fed to the patient that coats the esophagus and stomach with barium, and then X-rays are taken
● Upper endoscopy – An endoscope (long tube with a camera and light attached to the end) is inserted through the mouth and down the throat into the esophagus and then the stomach. The endoscope can also be used to remove abnormal tissue for biopsy.
● Serum pepsinogen test – A test that measures the levels of pepsinogen in the blood. Low levels of pepsinogen are a sign of chronic gastric atrophy which may lead to stomach cancer. This test doesn't screen for gastric cancer itself but it does screen for people who might be at high risk for gastric cancer.
Risk Factors for stomach cancer
● Age – Over 50
● Gender – Men are more likely to develop stomach cancer than women.
● Geographic location – Worldwide, stomach cancer is more common in Japan, China, Southern and Eastern Europe, and South and Central America. This disease is less common in Northern and Western Africa, South Central Asia, and North America.
● Helicobacter pylori infection - Helicobacter pylori (H pylori) bacteria seems to be a major cause of stomach cancer, especially cancers in the lower (distal) part of the stomach. Long-term infection of the stomach with this germ may lead to inflammation (called chronic atrophic gastritis) and pre-cancerous changes of the inner lining of the stomach.
■ People with stomach cancer have a higher rate of H pylori infection than people without this cancer. H pylori infection is also linked to some types of lymphoma of the stomach. Even so, most people who carry this germ in their stomach never develop cancer.
● Obesity/being overweight
● Tobacco Use – Rate of stomach cancers are almost doubled in smokers compared to nonsmokers.
● Diet - An increased risk of stomach cancer is seen in people with diets that have large amounts of smoked foods, salted fish and meat, and pickled vegetables. Nitrates and nitrites are substances commonly found in cured meats. They can be converted by certain bacteria, such as H pylori, into compounds that have been shown to cause stomach cancer in lab animals.
● Inherited conditions or attributes
■ A family history of stomach cancer
■ Type A blood – May lead to a very small increased risk
■ Familial adenomatous polyposis (FAP).
■ Hereditary nonpolyposis colon cancer (HNPCC; Lynch syndrome).
● Occupational Exposures – Working in the coal or rubber industries may lead to a small increase in risk for stomach cancer
● Radiation exposure
Protective Factors
These behaviors do not guarantee that you will not have stomach cancer, but engaging in them may reduce your risk for developing stomach cancer.
● Abstaining from or stopping smoking – Studies show that smoking increases the risk of stomach cancer, as well as many other cancers. Never smoking or stopping smoking can reduce your risk for stomach cancer.
● Treating Helicobacter pylori infection – A chronic H. pylori infection increases the risk of stomach cancer.
● Diet – Eating a diet rich in fruits and vegetables may help decrease the risk of stomach cancer, although the evidence is still inconclusive. Some studies have also found that eating many whole grains, carotenoids (found in carrots, sweet potatoes, dark leafy greens and other vegetables) and green tea may also reduce stomach cancer risk.
Treatment methods
Screening is rarely done for early stage Gastric cancer, and so most gastric cancer is diagnosed at a later stage when treatment might be more difficult.
● Surgery – the first line of treatment for stomach cancer.
■ If the cancer is diagnosed at an early enough stage, a procedure known as endoscopic resection can be used, where an endoscope is inserted into the stomach through the mouth, throat, and esophagus and used to cut out the tumor without removing much of the surrounding tissue.
■ This is more common in Japan, where a public, population based gastric cancer screening program leads to gastric cancer being diagnosed earlier. Where gastric cancer screening is less common it is usually diagnosed at later stages where this is not an option.
■ Later stage cancers typically require the removal of part or all of the stomach (subtotal or total gastrectomy). If a total gastrectomy is performed the esophagus will be attached to the small intestine to create another stomach.
● Chemotherapy – Cancer cell killing drugs may be administered either alongside surgery, to shrink the tumor so that it can be removed more easily. Chemotherapy may slow down or stop the growth of late stage stomach cancer if the patient is too ill for surgery, but will not force a cancer into remission on its own.
● Chemotherapy – Cancer cell killing drugs may be administered either alongside surgery, to shrink the tumor so that it can be removed more easily. Chemotherapy may slow down or stop the growth of late stage stomach cancer if the patient is too ill for surgery, but will not force a cancer into remission on its own.
● Chemotherapy – Cancer cell killing drugs may be administered either alongside surgery, to shrink the tumor so that it can be removed more easily. Chemotherapy may slow down or stop the growth of late stage stomach cancer if the patient is too ill for surgery, but will not force a cancer into remission on its own.
● Targeted Therapy – A monoclonal antibody, called trastuzamab or Herceptin, can be used to slow the growth of a subgroup late stage stomach cancer that overexpress the HER2 gene in their cells.
● Radiation Therapy – Radiotherapy is not normally used as a first line treatment for stomach cancer, but it is sometime used to ease the pain from advanced stomach cancer or to kill leftover cancer cells after a surgical resection of a tumor.
http://www.cancerresearchuk.org/cancer-help/type/stomach-cancer/about/stomach-cancer-risks-and-causes
http://www.cancer.gov/cancertopics/pdq/screening/gastric/Patient/page3